Despite how common pain and injury is in running, it is often difficult fo us runners to find a fast and effective solution.
Despite how common pain and injury is in running, it is often difficult fo us runners to find a fast and effective solution.
This may be due to the complexity of our issues, or it could be logistical. That’s because many trail runners and ultrarunners live in places with a bounty of beautiful sights, sounds, and landscapes, but a dearth of skilled medical resources.
The goal of most articles in Stay the Course is to either directly assist runners in self-improvement, or to illuminate the myriad possible factors that runners and their medical team should consider when addressing injury or pain. Our goal in this article is to provide a roadmap for dealing with chronic pain. We cover:
- How to self-intervene early;
- Seeking professional help when needed;
- Understanding what that help looks like; and
- How runners can be the best advocates for their injury recovery.
Stage 0: When to Seek Medical Attention for Acute and Worsening Pain
This guide is primarily for runners with chronic pain, whose symptoms are largely stable and functional. This means:
- The injury or dysfunction is more than a few days or weeks old (chronic pain is usually defined as unchanging pain for more than three months);
- The symptoms are consistent, usually related to activity; and
- The symptoms do not significantly interfere with non-running life.
This usually means that you have pain related to running or physical activity, that it may trickle into daily life — for example, you might have stiffness after inactivity, or minor symptoms with certain positions and activities — but you are still able to function.
It is imperative to seek medical attention if your pain presents differently, including as:
- Severe pain;
- Progressively worsening pain over the course of days or weeks;
- Pain that severely interferes with normal life functions such as sleeping, standing, sitting, or walking short distances; and
- Other symptoms of more acute, non-orthopedic issues such as night pain, unexplained weight loss, or bowel or bladder changes.
Stage 1: Do-It-Yourself Chronic Pain Mitigation
Most runners with a stubborn injury or pain will have tried a variety of strategies that might include:
- Seeing a doctor, and getting basic imaging such as x-rays;
- Self-treatment techniques like rest, ice, heat, stretching, or strength work; and
- Seeing a hands-on practitioner such as a massage therapist, chiropractor, or physiotherapist.
Yet, this often fails to resolve pain. Why? Often, those resources are missing key aspects of the pain equation.
Notably, the vast majority of running chronic pain issues are related to dysfunctions, not actual injury. True injuries are a result of actual tissue damage and/or an inflammatory response, whereas dysfunctions are related to pathological movement patterns such as too much, not enough, or inefficient movement.
Injuries heal with time, and pain related to that injury should subside when those tissues fully heal, usually in a few weeks. Dysfunctions often will not change until active effort and energy is placed into correcting that inefficient movement pattern: moving a bone, massaging or stretching a muscle. As such, it’s imperative for all runners to assess how they move.
Below are the steps in this do-it-yourself stage:
Rest
When in doubt, rest. While I seldom recommend this as a first resort, for the frustrated runner going at it alone, a small amount of rest is a key initial test. Even after 12 years as a medical professional, the number of chronically ailing runners who have tried every treatment intervention except rest still shocks me!
Start with a week off. Gauge the change of symptoms not just during the rest period, but in the days after a gradual return to running. If symptoms quickly regress upon return to small amounts of running, then it’s more likely there is a movement dysfunction present that is creating the pain. No amount of rest changes a movement problem.
Stride Efficiency
The next step is a running stride self-assessment. Film yourself running in both side and front views.
You may not be a stride expert but, when you watch the footage, does it look normal? More importantly, does it look like your normal? Is there an imbalance that wasn’t there before, or that has become more severe?
Our form plays the biggest role in how our body feels, both during and after the run. If something is off, that needs immediate correction. Consider some do-it-yourself corrections, which can be done step-wise, or simply by look and feel.
If a stride adjustment is neither warranted nor changes your pain, then you can continue or skip to Stages 2 or 3.

The author demonstrating neutral and forward trunk engagement with efficient hip extension and arm swing. Photo: Joe Uhan
Mobility Self-Assessment
Most medical professionals are not particularly skilled at running-specific mobility assessment. To self-assess – and gauge both overall quantity and symmetry – perform these performance mobility tests. Is there anything particularly stiff, imbalanced, or triggering of your symptoms?
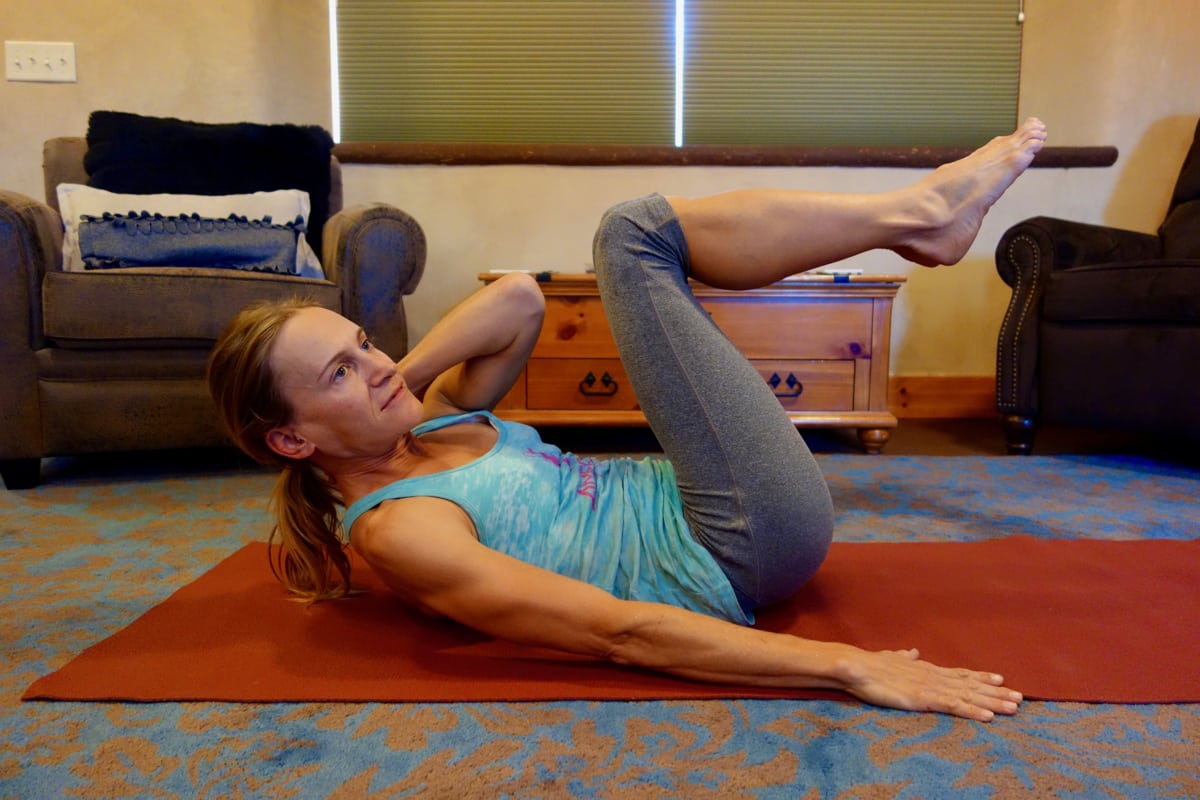
Core Activation
Efficient running requires both functional mobility and an active, efficient core stability system. The primary core muscles of interest include the deep abdomen (transverse abdominis), which holds our spine and pelvis steady while assisting upward hip flexion, as well as the glutes (and the deep hip rotators), which help to both stabilize the entire leg when we land and power the push off.
It is quite possible to run both far and pretty fast without an activated core. In a case like this, the hip flexors, quads, and hamstrings tend to over-work, and/or move the limbs less efficiently than if an activated core assists. Activation occurs when we actively use a muscle, and are able to feel a prolonged contraction.
Two key core activator exercises include the Diagonal Chop for the abs and Short and Long for the glutes. Try these exercises. If it requires a prolonged hold time (more than 10 to 20 seconds) to feel the abs and glutes burn, or if you can’t feel them at all, you may have core inhibition.
If so, focus on prolonged holds of these exercises before any attempt to run. If you have no luck in feeling the abs or glutes, you may have advanced mobility deficits or other issues preventing an efficient core. Proceed to Stage 3, as you’ll need professional assistance to help solve this issue.
At this stage, if you still cannot sustainably improve your flexibility, strength, or stride, it is time to move forward to the next stage of problem-solving.
Stage 2: Getting to the Root of Your Issue(s)
If you’re here at Stage 2, you’ve already determined that:
- Your injury is not serious and at risk for greater harm (after clearance from a medical professional);
- Your current medical team hasn’t been able to fully pinpoint the true source and/or an effective treatment strategy; and
- You have self-identified deficits in your stride, mobility, or strength that need work.
Before working with a physiotherapist, sports medicine physician, or hands-on practitioner, it’s often helpful to pause here in Stage 2 and gather more information.
If every injury seamlessly responded to rest; basic medical advice; and foundational mobility, strength, and stride efficiency; there would be far fewer injured — and frustrated — runners out there. But runners’ bodies are complex and treating a focal pain issue can be really challenging. As such, many medical professionals aren’t always equipped to fully and thoroughly assess the running body.
Before selecting your helper, here are three considerations to help you select the appropriate practitioner, ask them the right questions, and supply them with the more useful background information about you.
1. What Tissues Are Involved?
What are all the possible contributions to your running pain? This includes what tissues are actually painful, as well as any adjacent or systemic tissues that are directly or indirectly contributing to your pain.
A great many runners and sports medicine professionals believe runners can only experience pain from muscles, tendons, and bones, with the occasional tip toward joint pain.
Bu more tissues can hurt than just those. This can include connective tissue such as fascia — including the fascia around our guts that lay on top of our spine, pelvis, and hips — but also nerves, which are involved (in my professional experience) in about 75% of all chronic running pain cases.
You may not be able to tell that your pain is, say, from the sciatic nerve rather than a hamstring. But awareness of the possibility of nerve pain (through recognition of its signs and the different ways nerves can create chronic pain) will help steer you toward a helper with experience treating nerve pain.
Lastly, the final frontier for running pain and dysfunction is the pelvic floor. Weakness, tension, or combinations thereof affect not only the mobility and stability of the pelvis, but pelvic floor dysfunction can wreak havoc on the efficient function of the entire leg. Signs that the pelvic floor may be involved in a running injury could include bladder control issues (leakage or difficultly in smooth, relaxed voiding), pain during bowel movement or sexual activity, or any generalized pain in the perineal area. Even without noticeable symptoms, the pelvic floor should be evaluated in any chronically ailing runner.
2. System Interactions: “It’s all connected!”
If you determined from Stage 1 that you have motion or strength deficits, it’s important to consider how your whole body interacts may be playing a crucial role in creating and perpetuating your pain.
As such, it’s vital to select a sports medicine professional who takes a systems-based approach to treatment. This means they will examine your entire body and help determine if seemingly unrelated body areas may be conspiring.
For example, in my clinical practice, at least 25% of chronic “plantar” foot pain clients have nerve involvement where a nerve is either magnifying the pain or fully responsible for it. Of that group, half of them require cervical spine treatment to achieve full pain relief.
Thus, as you are selecting your helper, consider your whole body: are there other aches, pains, stiffnesses, or niggles that you are ignoring, because they seem less important and perhaps irrelevant to your running pain?
Moreover, do you have a trauma history? Have you experienced serious falls, accidents, surgeries, or other insults in the past that may impact an efficient running system?
If so, they may somehow be related to your running pain. As such, it’s wise to select a well-rounded – but still running-experienced – helper who can and will examine and treat your whole body.
3. Advanced Pain Complexity
What about the big picture? What larger issues might be playing a role in perpetuating pain?
Pain is complex, and often has both peripheral (local tissue) and central (brain) influences. Because the brain ultimately decides what is painful, non-orthopedic factors may perpetuate chronic pain. They include nutrition, stress, and sleep.
Being armed with these insights – about your body, your history, and the various systems and variables that could be impacting your pain – you’ll be far better prepared to select the appropriate helper, and provide them the best possible information to lead to a successful diagnosis and treatment.
On to Stage 3!
Stage 3: Bring On the Pros
If you’ve made it to this stage, you’re better prepared than about 90% of all chronically injured clients. You have an idea of your deficits, what it could be or isn’t, and useful information about your history and body.
Here are the four possible steps in selecting your help, and how to work toward a solution:
1. The Movement Experts
The best possible advice I have for a chronically injured runner – with whom serious tissue damage has been ruled out, who has stable but stubborn pain, and thus far has not improved — is to select a movement expert.
The most common movement experts are physiotherapists: they are the only profession whose standard training and daily practice involves assessment of both focal tissues and global movement patterns of their patients. That said, some doctors (like osteopaths or multi-dimensional sports medicine physicians), sports-oriented massage therapists, and other hands-on practitioners are also skilled in assessing and treating a moving system.
In addition to all the various tissue factors, chronic pain clients require constant balancing of the four dimensions of mobility, strength, efficiency, and pacing. Trust the movement expert who will acknowledge, assess and treat your whole body.

Ayoub Ahansal running in the heat of the Sahara Desert at the Trans Zagora Trail Morocco. Photo: iRunFar/Meghan Hicks
2. Advanced Diagnostics
If the systems-based work fails to garner significant improvement, it may be time for more information. This includes advanced imaging such as magnetic resonance imaging (MRI) and computed tomographic imaging (CT). The specifics of what they do are less important than the fact that they can take a deeper, and more detailed, multi-dimensional look at specific tissue.
Most chronic pain runners jump too quickly to advanced imaging. Because it is so specific, such imaging fails to consider systemic interactions (for instance, a foot MRI will not show an irritated nerve at the lumbar spine and sacrum).
More importantly, diagnostic imaging, while excellent at identifying serious (broken, torn, or bleeding) pathology, it often identifies common wear and tear that may have no correlation to the actual pain. As stated here before, MRIs will find tissue pathology in 30 to 50% of completely asymptomatic people.
It’s easy for a frustrated runner and motivated helper to jump to a more aggressive treatment strategy if advanced imaging is done before conservative and systems-wide evaluation and treatment.
That said, sometimes it is necessary. Failure to relieve pain may be one factor, but if your movement expert finds chronic deficits in tissue mobility, strength, and stability, or a stubborn inability to move efficiently, imaging may be necessary to identify what might be the culprit. Be aware of the utility of advanced imaging, but be aware of the downside, as well.
3. Advanced Restorative Options
Should conservative care fail to improve pain, and imaging finds (or fails to find) actionable pathology, there are more advanced restorative options for ailing runners.
While outside the scope of this article, other medical professionals – usually orthopedic specialist doctors – may be able to offer more potent anti-inflammatories such as local injections. Another strategy which is gaining both good clinical results and strong evidence is prolotherapy treatment. This involves the local injection of various agents ranging from sterile sugar water to blood platelets, to even stem cells to help facilitate healing of chronically dysfunctional and painful tissue.
4. Surgery: The Last but Often Necessary Resort
If you’ve made it this far and you’re still not better, I am truly sorry!
Surgery could include repairing torn tendons and ligaments. This often involves simply removing or cleaning irritated, unrepairable, and aggravated tissues from a joint or other body area.
It is often necessary, but sometimes is not. Occasionally, surgeries can make chronic pain worse. Thus, it’s important that both you and your medical team gather as much information and weigh all the possible benefits and risks – before making a decision.
A key factor in whether or not a surgery is warranted is if diagnostic imaging, or special (joint and tissue) loading tests, or the expert opinion of your team, believes that a specific structure is causing your pain. In such cases, a surgical intervention is more likely to be successful than if your team or doctor is less certain and wants to perform an exploratory procedure.
However small, surgeries represent traumas, and thus introduce more complexity (and potential dysfunction) to your body. As such, it’s important that potential surgical benefits will truly outweigh the costs.
Stage 4: If at First You Don’t Succeed, Try Again
Lastly, don’t give up. Frustrating as it may be, chronic pain often requires multiple trips through this pathway in order to get enough information, find the right help, and apply the right treatments with the precise order and timing. It’s not easy. But just because it hasn’t yet happened, doesn’t mean that it never well.
So keep learning about your body, helpful professionals, and new strategies. The best of us helpers are constantly learning, so keep your chin up, keep at it, and have faith that this exhaustive approach will pay off!
[Author’s Note: The contents of this column as well as the author’s comments are provided for general informational purposes only and are not intended as a substitute for professional medical advice. Seek medical care and clearance if you experience pain or injury prior to attempting any technique described below. Do not use the information on this website for diagnosing or treating any medical or health condition.]
Call for Comments
- Tell us about some of your injury journeys and what stage you’re at now.
- Do you have a lingering chronic injury that you’ve learned to live with at this point?
- If so, are there to-do items in this roadmap that you haven’t yet tried?