 Over the past year of working in Steamboat Springs, Colorado, I worked with a highly active — yet extraordinarily stiff — clientele!
Over the past year of working in Steamboat Springs, Colorado, I worked with a highly active — yet extraordinarily stiff — clientele!
Some of the stiffness was attributed to falls, bumps, and bangs while skiing, snowboarding, mountain biking, trail running or, simply, encountering ice or mud. While traumas big and small are no joke, and should be addressed and treated thoroughly to avoid long-term issues, there seemed to be another factor in the super-stiffness of many otherwise highly active mountain locals who had no trauma history.
These folks had stiff and immobile muscles, tendons, and joints. This was not just in the heavy movers like the hips, knees, and ankles, but also in the spine and more traditionally supple areas like the shoulders, thighs, and abdomen.
Moreover, they often presented with severe functional motion deficits. They were unable to touch their toes, fully turn and look behind them, or sometimes even stand up straight. This was despite a consistent activity regimen that included daily walking, cycling, and stretching and yoga routines.
It was puzzling: how do such active people, absent serious trauma, get so stiff? The answer, I found, was hidden in our tissue chemistry!

A short morning yoga practice can help maintain functional mobility in endurance runners. Photo: iRunFar/Meghan Hicks
The Chemistry of Mobility
As athletes, we tend to think of our tissues as solid structures: metal rods and wires that are pushed and pulled to create functional motion. And, when things get stiff, it is a matter of rods that perhaps fail to slide, glide, and bend, and wires that are too tight. We think the solution is to push and pull some more until the rods and wires properly move!
In reality, we are made up of living tissue that — in the healthy, efficient state — is both wet and warm! And both of those properties are crucial for efficient, athletic mobility, strength, and function.
Returning to our basic mechanical analogy, two key components of our rods-and-wires system are lubricant and heat. The lubricant allows the rods and wires to slide and glide with minimal friction, and the heat is the element that helps distribute that lubricant across all the parts.
Back to living human anatomy. There are two components of human lube: water and a compound called hyaluronic acid (HA). HA is a polysaccharide — a molecule consisting of multiple simple sugars — that is found between tissue layers, particularly between deep fascia — the connective tissue that encapsulates and separates muscles, tendons, and bones — and adjacent muscle.
HA, dissolved in the water surrounding all tissues, becomes a living lubricant that allows smooth sliding and gliding between adjacent muscles, tendons, and bones. This allows not only motion but also the shock absorption required for athletic movement. In this way, HA acts like the WD-40 of our orthopedic tissues!
Getting into the nuance of human cellular and tissue biochemistry is both beyond the scope of this article and unnecessary. But what is important to know is how lifestyle factors impact this crucial lubrication system:
- HA requires dilution in water for efficient lubrication.
- Both repetitive overuse and tissue dehydration can cause HA to lose its fluid base and become “sticky.”
Sticky HA is suspected to be a factor in myofascial pain (1). HA, absent enough water and loaded excessively with compressive and shearing forces placed upon muscles during, for instance, distance running, can instead become more like a sticky glue than a slippery lube!
Simply put, insufficient hydration and/or too much tissue load — two factors that often go hand-in-hand during ultramarathon training and racing — can cause tissues to stick together. Indeed, my clinical experience finds that deficits of tissue play — the relative motion between one tissue layer and its neighbor — to be a far more prominent issue in both functional stiffness and myofascial pain than a muscle or tendon being stiff or strained.
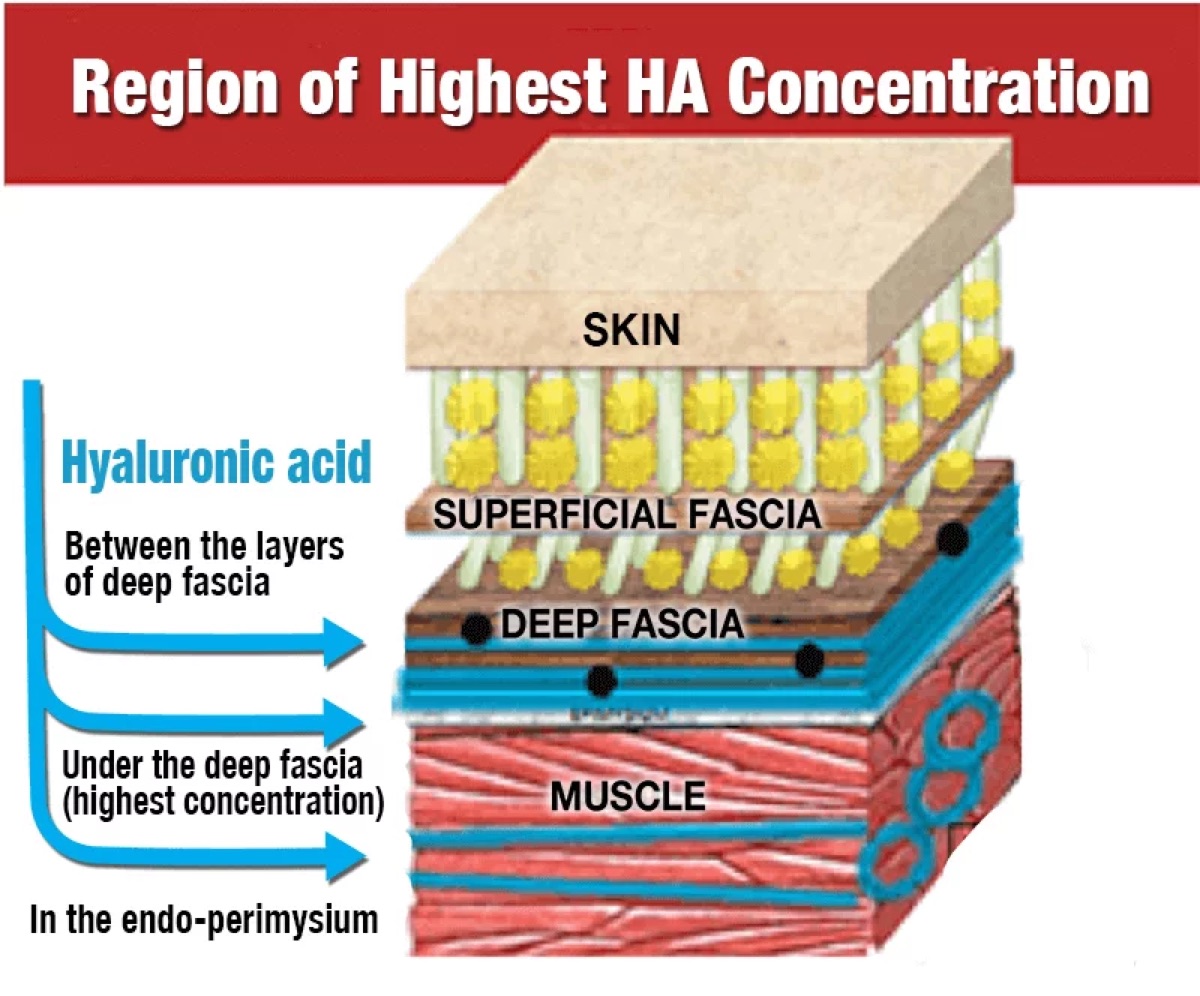
A graphic showing where hyaluronic acid should lie among human tissues. Image: Fasciafirstchiropractic.co.uk
The Problem: Life in a Cold and Dry Climate
This brings us back to my stiff mountain patients. If they were so active each day, why did they fail to maintain, let alone improve motion? The answer lies in a couple of lifestyle decisions.
Deficient Hydration
Steamboat Springs, Colorado, like much of the state, is relatively high alpine. Sitting at over 6,700 feet elevation, the sun is relatively strong and the climate quite dry. It is common for areas like these to boast a relative humidity under 20%. A strong sun, dry, blustery air, and an active lifestyle place huge demands on tissue hydration.
Nearly every client I worked with struggled to drink adequate volumes of fluid. When queried about hydration routines, two patterns emerged among my stiff clientele:
First, most folks began their nutritional day not with water, but with caffeinated beverages like coffee and tea. As a result, few of these stiff clients ingested non-caffeinated fluid until nearly lunchtime!
Second, most water consumption was back-loaded. They were more likely to drink water later in the day, with lunch or dinner, or after activity, rather than before. As such, their tissues were constantly playing catch-up.
Delayed Functional Mobility
The other factor that kept people stiff was that most people failed to do any significant physical activity until later in the day. A major factor in this decision is the morning cold.
Mountain towns can be downright chilly almost every morning, year-round. Even in the middle of summer, sunrise temperatures seldom break 40 degrees Fahrenheit. As such, many of my active clients were not morning exercisers. Most waited until late morning or later before they did any physical activity.
Instead, many of these otherwise active clients simply rolled out of bed and straight into a chair! This became even more of an issue, mid- and post-COVID-19 pandemic, where many lost the basic mobility routine of the office commute. Indeed, my very stiffest clients would frequently wake up, and within a few minutes be seated at a computer to work, often not moving again for several hours!
These combined factors sustained and exacerbated tissue stiffness at a chemical and cellular level. Even when these folks eventually did go for a walk, bike ride, or other activity at mid-day, their tissues had by then been significantly dehydrated and gone several daytime hours without any motion.
In this situation, at best they failed to generate or restore tissue mobility. At worst, they incurred myofascial pain, secondary to the sticky lubricant, resulting from inadequate hydration and a lack of movement earlier in the day.

Staying hydrated throughout the day, not just during and right after running, is crucial for our health. Here, David Sinclair rehydrates following the 2022 Canyons by UTMB 100k. Photo: iRunFar/Meghan Hicks
The Solution: Morning Mobility and Hydration
A key aspect of a comprehensive treatment plan for mobility deficits and/or myofascial pain is a morning mobility routine. I instruct all my stiff clients that, within 30 minutes of waking, they need to embark on a basic mobility exercise routine.
This may include a variety of elements, including (in order, from least to most aggressive):
- Foam rolling. This may be the easiest starting point for a sleepy person new to a morning routine: laying on a roller and performing slow, gentle movements to the spine and extremity muscle groups.
- Yoga. A gentle flow of movements to the spine and extremities is a great way to jump-start movement in a progressive and non-aggressive way.
- Running-specific dynamic stretching. This is a great strategy for the runners who tend to roll out of bed and are running within a few minutes of waking up. Generate tissue and fluid motion with running-specific movements.
- Running drills.
What this morning mobility routine does:
- Distributes hydration to tissues. Rolling and stretching do more than massage and stretch. It compresses and tensions tissue. In doing so, the tissues behave like sponges, absorbing and redistributing that extracellular fluid and HA within each muscle and throughout the system.
- Builds heat! A dynamic warm-up routine, even one of very low intensity, works to heat cold, stiff tissue. Indeed, a key remediation factor for sticky, dehydrated HA is the heat that comes from the progressive soft tissue mobilization of massage and dynamic stretching.
I begin all stiff clients on a basic foam rolling and dynamic, yoga-like stretching routine designed to take less than 15 minutes. If they choose not to then engage in exercise — walking, running, hiking, biking, or otherwise — that’s okay. The key is to jump-start tissue mobility before beginning the work day.
As for hydration:
- Begin each morning with at least 16 ounces of water.
- Amp up exercise hydration. Even if you’ve hydrated during your day, consider another pre-activity pint of water, as well as carrying supplemental fluid, especially if that outing is over an hour long and in warm and dry conditions.
In the morning, this water may have calories or electrolytes, but it should be uncaffeinated and in addition to any caffeine. It’s important to realize that we lose a tremendous amount of hydration overnight, during sleep. As such, jump-starting the day with a full pint of water — regardless of impending activity — allows for tissues to immediately begin reabsorbing water and preparing the tissues for whatever activity may be in store.
Then, prime your system again preceding your activity with another pint of water. This will at least cover any subtle deficit incurred during the day. Avoiding spikes in dehydration, even in the absence of thirst, may be a key in keeping that HA wet and slippery, and avoiding the dehydration stick.
In summary, tissues are healthiest, most mobile, and most efficient if they begin fully hydrated and stay that way!

Foam rolling for a few minutes in the morning can help to keep you mobile and your body tissues lubricated. Photo: iRunFar/Bryon Powell
Conclusion
Recognizing both the chemistry and timing of tissue mobility is crucial to maintaining and promoting mobility, as well as preparing our athletic system to be its best, at the very beginning of each day.
Keep that system primed and lubricated with an early watering of fluid and a sizable dose of mobility each morning and the rest of your day will feel and function a lot better!
Call for Comments
- Do you have a morning mobility and hydration routine? If so, leave a comment to share yours.
- Have you found that activity early in the day makes your body feel better than waiting until later on to exercise?
Reference
- https://www.mdpi.com/1422-0067/22/13/6845/htm . “Hyaluronan and the Fascial Frontier”, Pratt, R. International Journal of Molecular Science. 2021, 22(13), 6845
