It was the coldest part of the morning as Lori headed down toward the Beaver Mountain Lodge aid station during The Bear 100 Mile last fall. With temperatures hovering in the teens and low twenties Fahrenheit, you have to be quick or the warmth of the building will keep you inside, and so she forged on, 75-plus miles in. After a quick descent, the trail climbs steadily for 1,600 feet, one of the final few punches that come at Bear runners in the last 20 miles of the race. As the trail flattened out before the last push to the Beaver Creek summit and she tried to switch to a run, Lori realized that she wasn’t just breathing hard from the climb, she was struggling to breathe at all.
Thinking it might be compounded by dehydration, she consciously took in more fluids and thought about another runner she had met 30 miles earlier who ended his race at mile 50 due to asthma-like symptoms that had “come out of nowhere.” What was going on? Lori had previously been tested for asthma and exercise-induced bronchoconstriction, or tightening of the smooth muscles of the airways, without conclusive results. She is also an experienced ultrarunner who had never had this type of wheezing constriction before. She was smart, she didn’t panic (although that might just be ultra brain), and she limited her running to the downhills where the wheeze and discomfort were most manageable. Since that day last September, she’s had no other breathing issues while running or racing, but with more high-altitude 100 milers on the horizon it’s something still on her mind.
Since the 1980s, there have been a multitude of terms coined in an effort to describe the asthma-like symptoms that plague many athletes like exercise-induced asthma, skier’s asthma, hockey hack, cold-induced asthma, exercise-induced hyper-reactivity syndrome, and a new one to me, the Hardrock [100] cough (1). For years, research was focused on winter athletes training and racing in primarily cold conditions when these asthma-like symptoms most commonly arose. An entire theory emerged based on the cold taxing our respiratory system, and the scientific community ran with that explanation of events for a long time.
However, it soon became apparent that athletes exercising in hot, dry, and even indoor environments were also experiencing these asthma-like symptoms without a corresponding clinical asthma diagnosis. What we now know is that there are at least two main respiratory conditions that affect winter and summer athletes alike. These fall outside of an asthma diagnosis and are classified as airway dysfunction. These conditions are most commonly called exercise-induced bronchoconstriction (EIB) (which was formerly known as exercise-induced asthma), exercise-induced laryngeal obstruction (EILO) (formerly known as vocal-cord dysfunction), and high-altitude cough (HAC).
There is one more condition that has been recognized by the medical directors at the Hardrock 100 that mimics EIB and presents very similarly to what Lori experienced last year at The Bear. At this time its pathophysiology remains unknown, which places it squarely in its own category. For the time being, it’s simply, ‘a pulmonary experience of the Hardrock 100,’ and it’s fascinating!
The purpose of this article is to dive deeper into what EIB, EILO, and HAC are, risk factors for developing airway dysfunction, and how those factors play into our day-to-day lives as ultrarunners. As always, if you believe you have a respiratory condition, please seek medical assistance from your health-care provider. I do encourage you to comment to this article about your personal experience, too, since connecting with other runners who experience similar pulmonary events helps share our collective knowledge.
What is Exercise-Induced Bronchoconstriction?
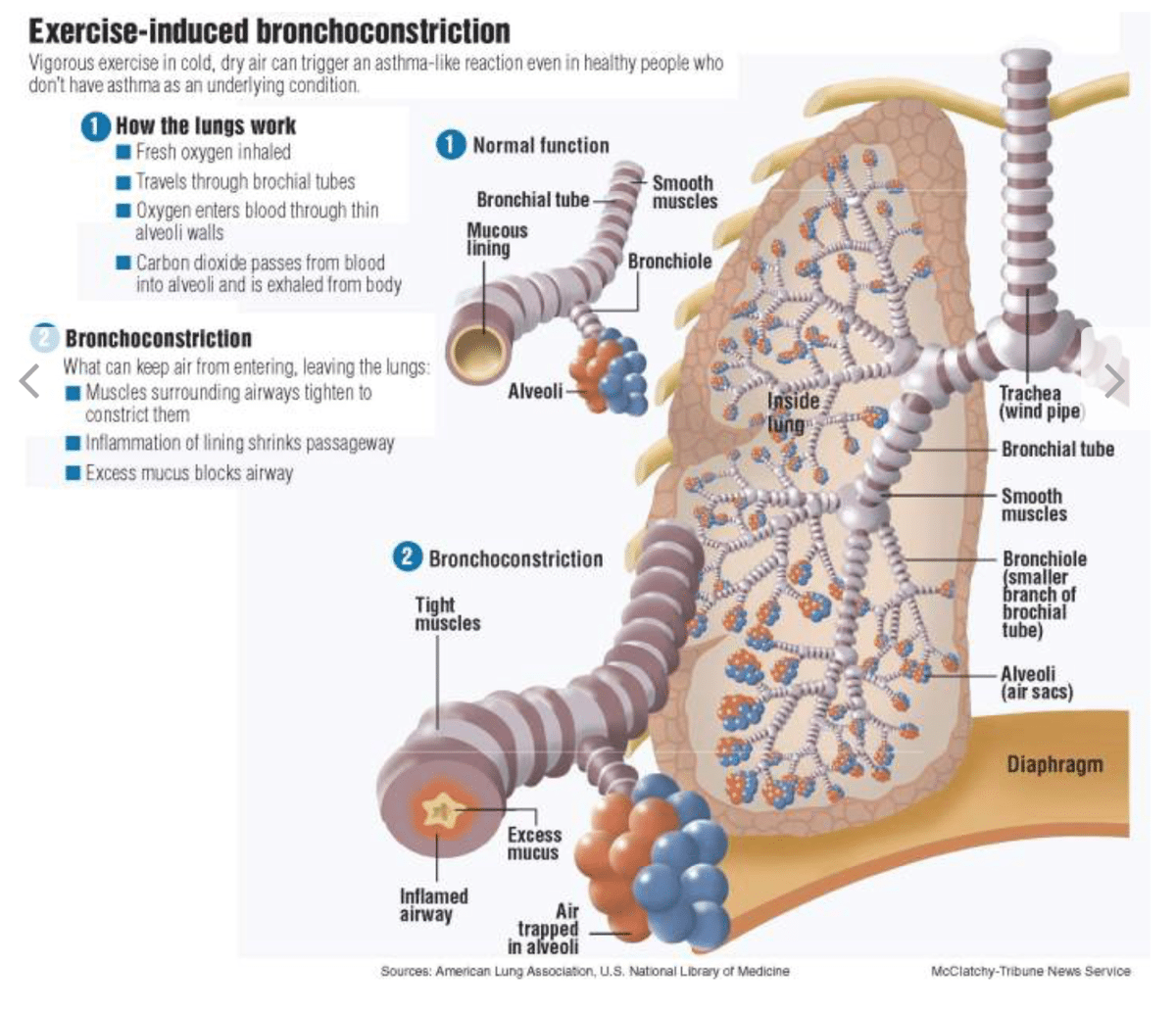
Exercise-induced bronchoconstriction (EIB) is a condition that can occur during or more commonly up to about 15 minutes post-exercise. During exercise, there is an increase in ventilation, the rate at which you are breathing, and in certain individuals there is a subsequent narrowing of the bronchi and bronchioles, the branches of the air passages in your lungs, causing a restriction of airflow (2). Previously known as exercise-induced asthma, as it was once believed to be most prevalent in the asthmatic population, it is now clear that EIB symptoms are not always consistent with classical chronic asthma (1). Essentially, many athletes who have asthma may experience EIB, but not everyone who experiences EIB has asthma.
When you exercise and you’re breathing hard and fast, this causes water evaporation of the airway surface liquid that makes up the lining of your bronchioles. This causes a shift in osmotic gradient, or the movement of liquid, during and post-exercise, which stimulates the release of inflammatory mediators. Inflammatory mediators, like histamine, can influence the bronchial smooth muscle and cause constriction, mucus build-up, and edema (1). It’s believed this occurs due to excessive calcium being released as cells shrink due to the shift in osmotic gradients in response to the increased evaporation occurring during exercise.
Although more prevalent in winter athletes, EIB is not exclusively a winter-athlete problem. Although cold, dry air is the most widely-talked-about cause, pollutants, allergens, particulate matter, nitrogen oxides, and the ozone pose equally adverse threats when ventilation is increased during exercise. Olympic swimmers exposed to chlorinated pools, speed skaters and hockey players exposed to ice-resurfacing-machine fumes, and cyclists exposed to a wide variety of air particulates on the road report a prevalence of EIB equal to or greater than the rates seen in the most traditional EIB-causing sport, cross-country skiing (3). This is relevant to runners training through brutally cold winter months, wildfire-smoke-filled summer months, inversions trapping pollutants and causing poor air quality, and many other potentially adverse training and racing environments.
The concern is that repeated exposures to cold, dry, irritant-filled air has been shown to cause a remodeling of the parts of the lungs’ basement membrane, causing an increase in thickness of these membranes (3). When this occurs, the body has a reduced capacity to respond to water loss of the airway liquid surface by evaporation (1). It is believed that this chronic exposure to cold and/or dry air and the subsequent remodeling of the airway may in fact be irreversible, leading to a chronic and worsening EIB.
The demands we, as endurance-driven athletes, place on our pulmonary systems are immense, sometimes exceeding the capacity of that system. Even the slightest impairment to the pulmonary and/or respiratory system can result in large performance decreases (4). Airway inflammation and airway limitation appear to progressively develop over a lifetime in many endurance athletes, with 90% of the asthmatic population and 20% of the general population developing EIB (1,3,12). The progressive nature of EIB ultimately leads to a ventilatory limitation during performance as a result of airway-structure changes due to frequent environmental exposure (4).
In many ways, think of EIB as an overuse injury of the lungs. What I mean by this is that, generally speaking, though the cells that line our airways have a great capacity to repair themselves quickly, it’s a repeated injury-repair cycle that is believed to be responsible for the airway’s permanent structural changes. This is a slow but progressive process. There are certainly factors that may predispose us to developing EIB including high-intensity activities, history of asthma, allergies, a history of atopy (or being hyperallergic), and allergic rhinitis (an allergic reaction to airborne allergens) (13). Additionally, the environmental conditions we regularly train and race in are known risk factors including cold air, dry air, high pollen counts, pollution, insecticides, fertilizers, wildfire smoke, chlorination, car exhaust, and more (13).
What is Exercise-Induced Laryngeal Obstruction?
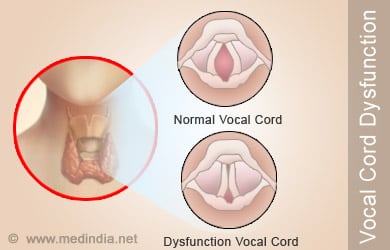
Exercise-induced laryngeal obstruction (EILO) is defined by a shortness of breath on exertion caused by the inappropriate narrowing of the larynx during high-intensity exercise, which can become more prevalent in stressful situations. The larynx is a part of the respiratory system that both holds the vocal cords and allows air to pass between the mouth and the trachea and onto the lungs (and back again). EILO is most often characterized by its prototypical inspiratory stridor or, a high-pitched whistling noise heard on inhalation (5). Many of those experiencing EILO also complain of accompanying chest and/or throat pain that occurs because the vocal cords are adducting, or closing, during inspiration when they should instead be abducting, or opening, to allow for minimal obstruction of air flow as you inhale (6).
Complete abduction of laryngeal structures is normal and required during exercise to optimize maximum airflow when you inhale. When abnormal adduction of these structures occurs, turbulent airflow and increased resistance of the inhaled air results. At the extreme end of this abnormal closing of the vocal cords, you suddenly have a wheezing athlete who is short of breath as they try unsuccessfully to inhale properly (7).
EILO is most commonly diagnosed during adolescence, but is also seen in the adult population. Exact numbers are unknown as EILO until recently has been frequently misdiagnosed as other breathing conditions. This is due to improper clinical testing practices that couldn’t differentiate between asthma and other dysfunctional respiratory conditions (7). This has led to much discussion on how healthcare practitioners can differentiate between asthma, EIB, and EILO in a clinical setting.
In the field, general diagnosis can rely on the timing of the onset of the pulmonary episode and how/if the condition subsides. Most simply, unlike EIB, which comes on more commonly on cessation of exercise or with a decrease in exercise intensity (change in ventilation rate), EILO generally occurs during peak intensity and will subside on its own within three to five minutes of cessation of activity (7, 5).
Additionally, EILO rarely responds solely to the use of a therapeutic inhaler. Successful treatment of EILO with an inhaler is likely the result of relieving the panic and anxiety occurring during the episode, and is effective in getting the athlete to calm down. Therapeutic ‘reliever’ inhalers work as bronchodilators designed to abate the spasms of the airway muscles restricting airflow during an asthma attack and therefore do not physiologically affect the cause of EILO. In fact, EILO is most successfully treated with breathing exercises, which alter the rate and intensity of your inhalations, including inhaling through pursed lips or forcefully through your teeth.
Anecdotally, I have witnessed medical staff treating an episode of EILO in the field by having the athlete inhale through a plastic straw. The interesting thing about EILO is that although we are developing effective ways to treat it, as of 2017, its cause still remains relatively unknown. Conditions often linked to EILO include chronic cough, globus (or the sensation of having a lump in your throat), gastroesophageal reflux disease (the movement of stomach acid up into your esophagus), neurological voice disorders, and hyper reactivity of the laryngeal bodies caused by allergies and infections (9,10). Interestingly, there is also thought to be a psychological link to EILO episodes. What this means generally is that stress and anxiety increases the likelihood of an episode reoccurring, and not that EILO is tied to any specific psychiatric conditions (10). Curiously, EILO seems to present more commonly in female athletes with roughly 68% of documented cases being female (14).
Unlike clinical asthma, because both EIB and EILO happen in association with exercise, doing a functional exercise test is the best way to get an accurate diagnosis. There are many different varieties of these tests but the key difference is that if the timing of symptoms corresponds more closely with EILO, then the exercise testing needs to be done via a continuous laryngoscopy exercise (CLE) test. A CLE test utilizes a flexible laryngoscope, most commonly a nasal endoscope, that this fixed to head gear and allows for continuous video of laryngeal movement during exercise to take place. This allows for the clearest possible picture into a physical cause of respiratory dysfunction.
What is High-Altitude Cough?
Another common respiratory culprit is the high-altitude cough (HAC). Unlike the other two respiratory dysfunctions we’ve talked about, HAC is truly limited to one specific cause, high elevations. Most of the current scientific literature focuses on mountaineers in the Khumbu region of Nepal, because HAC is most commonly seen above 5,000 meters (16,400 feet) altitude with increasing severity as mountaineers ascend to higher elevation. However, HAC is an accompanying symptom of acute mountain sickness that effects as many as 30 to 45% of people at elevations as low as 3,500 to 4,500 meters (11,500 to 14,750 feet) and is compounded by the intensity at which the person is moving (11). This would suggest that even outside of Mount Everest’s environs, given the intensity of running an ultramarathon, seeing HAC at many of our high-altitude ultras is not implausible. In fact, in talks with one of the medical directors for the Hardrock 100, Steve Halvorson, MD, he says that many Hardrock participants develop this very same coughing experience each year.
In both cases of either the dreaded ‘Khumbu cough’ or ‘Hardrock cough,’ mountaineers and runners alike develop a nonproductive cough likely caused by the interaction of several variables. For a long time, it was believed that the cold, dry air found in these mountain environments was the main culprit, similar to EIB. This same cough is not as frequently seen in a chronic manner in lower-altitude, cold, dry activities. Similar to EIB, it is believed one of the chief causative agents is likely water loss from the respiratory tract via evaporation. However, unlike EIB, other possible causes include sub-clinical pulmonary edema, fluid in the lungs, and—similar to EILO—an additional possible cause is gastroesophageal reflux disease (11).
At this point, the exact cause is unknown and it is clear that within in a few days of returning to lower elevation the cough subsides on its own. In most cases, HAC does not seem to have any effects on performance during ultramarathons other than being annoying, though several cases of broken ribs have been documented in mountaineers who are exposed to high-altitude conditions and have this cough for more extended periods of time.
What is Happening at the Hardrock 100?
Now, what the heck is going on at Hardrock? Having spoken with numerous athletes who have collectively toed the line at The Bear, Run Rabbit Run 100 Mile, Wasatch Front 100 Mile, Hardrock, and Leadville Trail 100 Mile, they have all experienced a combination of one-off and recurrent pulmonary episodes. While recurrent episodes are likely EIB, EILO, or asthma, one-off episodes are inherently curious in their sudden and seemingly unpredictable occurrence.
Having heard whispers of this being a particularly common occurrence at the Hardrock 100, I reached out to one of the medical directors for the event, Steve Halvorson, MD. Steve has seen HAC and high-altitude pulmonary events first hand, having helped with high-altitude and HAC research at the Everest basecamp in 2010. When asked about the episodes they’ve seen at Hardrock over the years, he believes, from reviewing the literature and speaking with other medical directors, that the prevalence of pulmonary complaints and drops because of pulmonary episodes seem to be higher at Hardrock, and thus unique in comparison to other races. This is likely due to the extent of the race that takes place at or above 11,000 feet (3,350 meters) altitude as it would exacerbate the ventilation rate and duration at which the runner is breathing hard. Additionally, because of the race’s location, environmentally, it presents many irritants for an athlete’s respiratory tract.
Steve and his co-medical director, Geoff Clover, MD, have done an excellent job of drilling down on confounding variables when runners present with pulmonary episodes during Hardrock. By asking questions about the athlete’s history of asthma, reactive-airway disease, EIB, time spent acclimatizing, history of similar problems, recent viral infection (a potential trigger for HAC), and history of high-altitude pulmonary edema (HAPE), they hope to get a better picture of potential causes of these seemingly ultrarunning-at-high-altitude-specific episodes.
When examining these preceding variables and their associated symptoms (presence of cough, rales, wheezes, or stridor), there appears to be a lot of overlap with EIB, HAC, EILO, and HAPE. What we don’t yet know is if these pulmonary episodes are occurring at the bronchioles or further up the respiratory tract. The other unknown, fascinating component is that it appears that running for this long in adverse environments is powerful enough to cause a previously asthma-free, EIB-free athlete to experience what at the very least mimics EIB in every way other than it being a one-time event. The implications of this are captivating because of the fact that we do not yet have the answers, and neither does the scientific literature. What does that mean for us, the ultrarunners? It means we get to be at the forefront of wilderness medicine, so help the good doctors out, and breathe deep for me.
What You Should Know on the Trail or in a Race
This article is not intended to be alarmist or fear mongering, or make you rush to schedule an appointment with your primary-care provider. My intention is to add context to situations you might find yourself or your fellow racers experiencing. So what should you do if you are struggling to breathe during a run or race?
One, don’t panic! This is where I picture my friend’s mom yelling at me, “But I’m trying so hard to relax!” Ask for help from a fellow trail user or medical volunteer at an aid station. People are there to help. As mentioned earlier, panic will worsen episodes of EILO, so breathe slowly through pursed lips or through your teeth as you evaluate your situation.
Two, identify the timing and context of your breathing issues. Although we did not cover every possible medical cause of respiratory issues in this article, when it comes to EIB and EILO, the timing of the onset of symptoms and the timing of how they resolve is largely indicative of which might be the likely culprit in your shortness of breath. Simply remember: onset post-activity or intensity easing off with a long recovery of symptoms point toward EIB, and onset during activity and quickly resolving (one to five minutes) once stopping activity is more likely EILO.
Third, ask yourself if your symptoms recurrent and happening regularly after certain activities or during particular weather patterns. If you are noticing any serious continuing or worsening respiratory symptoms, I encourage you to address these concerns with your primary-care provider.
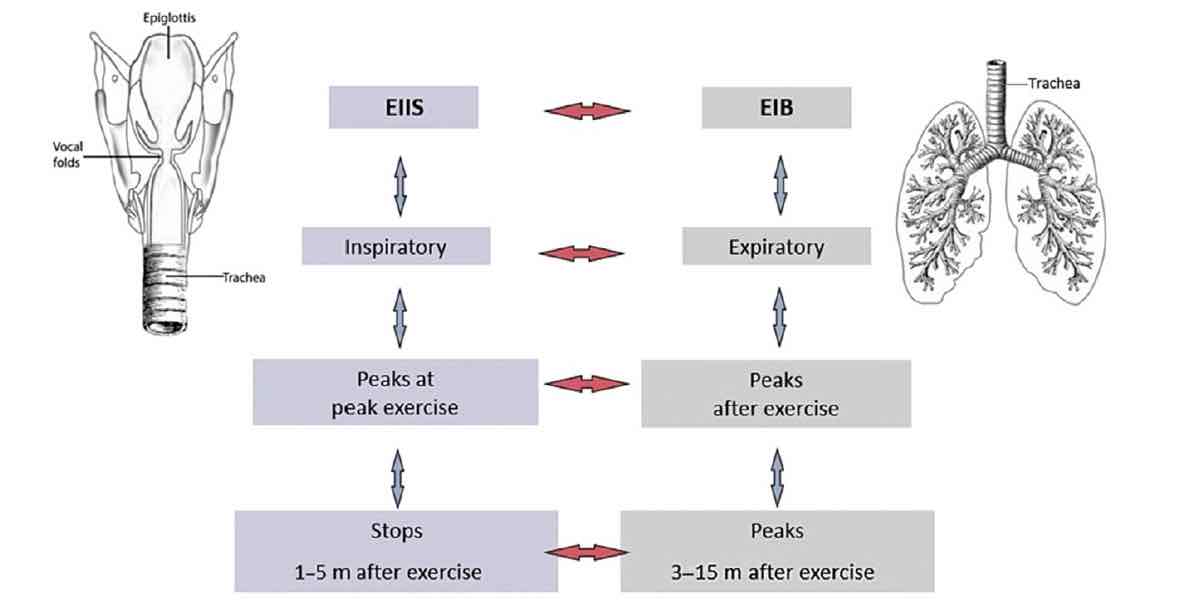
The characteristics of exercise-induced inspiratory symptoms versus exercise-induced bronchiorestriction. Image: Røksund, O. D., Heimdal J.H., Clemm H., et al. Exercise inducible laryngeal obstruction diagnostics and management. Paediatr Respir Rev 2017;21:87
Call for Comments (from Meghan)
- Have you been diagnosed with non-asthma airway dysfunction that occurs as part of your running and/or elsewhere in life? Can you share your story?
- Are you a medical practitioner who has seen endurance-running-associated breathing problems that aren’t asthma? Can you share your observations and what you’ve learned?
References
- Rundell, K., & Jenkinson, D. (2002). Exercise-induced Bronchospasm in the Elite Athlete. Sports Medicine, 583-600.
- Parsons, J., Hallstrand, T., Mastronarde, J., Kaminsky, D., Rundell, K., James, H., Storms, W., Weiler, J., Cheek, F., Wilson, K., & Anderson, SD. (2013). An Official American Thoracic Society Clinical Practice Guideline: Exercise-induced Bronchoconstriction. American Thoracic Society Documents.
- Kippelen, P., Fitch, K., Anderson, S., Bougault, V., Boulet, L., Rundell, K., Malcolm, S., & Mckenzie, D. (2012). Respiratory health of elite athletes- preventing airway injury: A critical review. British Journal of Sports Medicine, 471-476.
- Sheel, A., Macnutt, M., & Querido, J. (2010). The pulmonary system during exercise in hypoxia and the cold. Experimental Physiology, 422-430.
- Røksund, O. D., Olin, J. T., & Halvorsen, T. (2018). Working Towards a Common Transatlantic Approach for Evaluation of Exercise-Induced Laryngeal Obstruction. Immunology and Allergy Clinics of North America,38(2), 281-292. doi:10.1016/j.iac.2018.01.002
- Weinberger, M., & Doshi, D. (2017). Vocal cord dysfunction: A functional cause of respiratory distress. Breathe,13(1), 15-21. doi:10.1183/20734735.019316
- Hall, A., Thomas, M., Sandhu, G., & Hull, J. H. (2016). Exercise-induced laryngeal obstruction: A common and overlooked cause of exertional breathlessness. British Journal of General Practice,66(650). doi:10.3399/bjgp16x687001
- Graham, S., Deardorff, E., Johnston, K., & Olin, J. T. (2017). The Fortuitous Discovery of the Olin EILOBI Breathing Techniques: A Case Study. Journal of Voice. doi:10.1016/j.jvoice.2017.08.019
- Morrison, M., Rammage, L., & Emami, A. (1999). The irritable larynx syndrome. Journal of Voice,13(3), 447-455. doi:10.1016/s0892-1997(99)80049-6
- Røksund, O. D., Heimdal, J., Olofsson, J., Maat, R. C., & Halvorsen, T. (2014). Larynx during exercise: The unexplored bottleneck of the airways.European Archives of Oto-Rhino-Laryngology,272(9), 2101-2109. doi:10.1007/s00405-014-3159-3
- Mason, N. P. (2013). Altitude-related cough.Cough,9(1), 23. doi:10.1186/1745-9974-9-23
- Boulet, L. (2012). Cough and upper airway disorders in elite athletes a critical review. British Journal of Sports Medicine, 46(4), 417-21.
- Molis, M. A., & Molis, W. E. (2010). Exercise-Induced Bronchospasm.Sports Health: A Multidisciplinary Approach,2(4), 311-317. doi:10.1177/1941738110373735
- Maat, R. C., Hilland, M., Røksund, O. D., Halvorsen, T., Olofsson, J., Aarstad, H. J., & Heimdal, J. (2011). Exercise-induced laryngeal obstruction: Natural history and effect of surgical treatment.European Archives of Oto-Rhino-Laryngology,268(10), 1485-1492. doi:10.1007/s00405-011-1656-1