 As I write this, I am about to test to become a Certified Functional Manual Therapist. The certification, which tests on eight different manual physical therapy courses, covers an enormous breadth of material ranging from the big toe to the skull. By the time this article is published, I will have either passed or failed. Either way, I have learned a tremendous amount about the human body, not simply the nuts and bolts–the bones and muscles–but the whole system’s interconnectedness. I have learned about tissues and structures that, fresh out of school, I thought had no bearing on daily life or athletic function, but actually do. In fact, what I love about Functional Manual Therapy (FMT) is its holistic, systems-based approach to optimal health and function.
As I write this, I am about to test to become a Certified Functional Manual Therapist. The certification, which tests on eight different manual physical therapy courses, covers an enormous breadth of material ranging from the big toe to the skull. By the time this article is published, I will have either passed or failed. Either way, I have learned a tremendous amount about the human body, not simply the nuts and bolts–the bones and muscles–but the whole system’s interconnectedness. I have learned about tissues and structures that, fresh out of school, I thought had no bearing on daily life or athletic function, but actually do. In fact, what I love about Functional Manual Therapy (FMT) is its holistic, systems-based approach to optimal health and function.
Of course, once Pandora’s box opens, things can get uncomfortable. In acknowledging that ‘everything matters,’ one must address areas and structures that, as a physical therapist who treats runners, you never thought you’d mention or treat. Chief among them is the coccyx. The coccyx, often referred to as the ‘tailbone,’ sits at the very tip (or inferior end) of the spinal column. It’s beneath the sacrum and, ahem, “in the superior gluteal cleft.” In ultrarunner translation, that’s the top of the butt crack!
Why should we as runners or medical professionals care about a little bone at the bottom of the spinal column that many have deemed a useless vestige of our evolutionary, tail-wagging days? It begins with folks who actually experience coccygeal pain and its debilitating effects. The impact of the coccyx goes beyond pain, though, and into hugely impactful realms of functional mobility, core stability, and pelvic-floor health.
What follows in this article is a brief primer on the coccyx: why you should care about it, how it can impact your running, and how to treat an injury of it.
The Tailbone: An Anatomy Review
The human spinal column consists of 22 separate bones: cervical, thoracic and lumbar. Below that is the sacrum, which is actually five bones that, over our evolution, have become fused into one large, triangular-shaped bone. At the very bottom of it all sits the coccyx. For most of us, it is the size of a nickel and consists of four tiny bones that, like its big brother the sacrum, are fused in a miniature triangle shape.
Like all the other bones in the spine, the coccyx can and should move. It has an efficient, neutral positioning that is susceptible to inefficiency. A coccyx becoming stuck or bent out of shape can have remarkable effects throughout our body. While it doesn’t seem like much, this little bone at the tail end of our spine is incredibly consequential to our function and athleticism as runners.
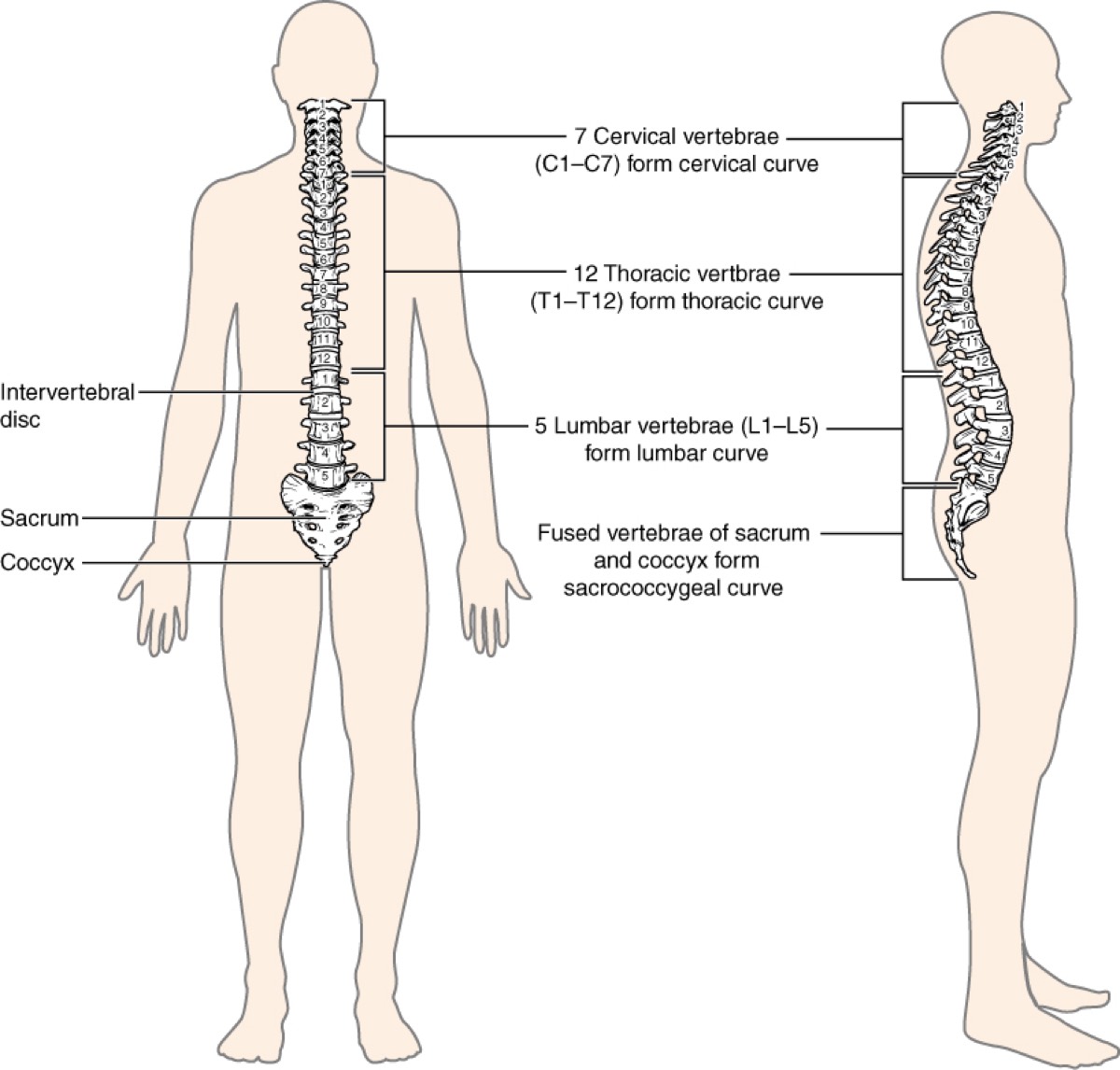
The vertebral column with the sacrum and coccyx at the bottom. Image: OpenStax College
Why the Coccyx Matters
The coccyx, due in part to its location and connections, is a crucial structure for two primary reasons:
1. The coccyx is the keystone of our pelvic floor.
The pelvic floor refers to the collection of small muscles that make up the core-stability system at the bottom of our pelvis. It is a hugely important system for function and athleticism. The pelvic floor has to, among other things, hold the weight of our guts, coordinate pelvic movement, and allow for the transit of things out of it!
Implication – Every pelvic-floor muscle has either direct or indirect attachments to the coccyx. As such, coccyx mobility loss or malalignment can cause significant pelvic-floor and core-stability dysfunction. This includes weakness, hypertonicity (too stiff and tight), or both–where one side is weak and the other tight. And while the topic of pelvic-floor health is deserving of an entire column on its own, suffice it to say that coccygeal inefficiency can significantly impair pelvic-floor (and whole-system core-stability) function.
2. The nervous system attaches to the coccyx.
The nervous system also connects to the coccyx. The spinal cord has a thin fascial layer around it called the dura mater. If you imagine that the nerves are electrical cables, then the dura is a loose plastic sheath around the wiring. As the spinal cord flows down through spinal column, the connective-tissue sheath of the dura attaches to the tip of the coccyx.
Implication – Coccyx stiffness or malalignment can cause pervasive range-of-motion restriction. Nerves need to move freely through our tissues in order to have full, pain-free mobility and optimal function. Restriction of any part of the nerve (including its outer sheath) can cause motion loss elsewhere in the system that is often unaffected by stretching until the coccyx is treated.
These core-stability and mobility factors that, if impaired by coccyx dysfunction, can cause systemic issues. In most cases, no amount of strengthening or stretching can overcome a dysfunctional coccyx. As such, it is the keystone structure to address in an FMT treatment approach. Without addressing any coccyx dysfunction, it may not be possible to get sustained improvement in strength, stability, range of motion, and pain relief.
It’s a small bone, but a big deal!
How a Coccyx Gets Dysfunctional
The most common cause of coccyx dysfunction is trauma. Simply falling on your butt is enough to cause either a mobility or alignment fault in the coccyx that, once sustained, usually will not self-correct without treatment. Pregnancy and childbirth are other potential causes of coccygeal dysfunction, as the fetus can push or pull the coccyx out of its optimal alignment. Postural and movement imbalances can also cause coccyx inefficiency. Impairments in how we stand, sit, and move can, over time, stiffen or torque the coccyx out of its efficient state.
How to Assess a Coccyx
Because the coccyx is at the top of the gluteal cleft, it can be uncomfortable for both the patient and manual therapist to assess. Here’s how an assessment usually goes:
- The best way to easily assess the coccyx is over skin, from top down, from below the pants or underwear.
- It is possible to both palpate and treat over loose-fitting athletic clothing. (This is my preference.)
- The coccyx can be assessed and treated without accessing any orifice.
- A skilled manual therapist can determine coccyx mobility and alignment, namely whether it is shifted forward or back, flexed or extended, and sidebent or rotated. Self-assessment is possible but more difficult, and requires skill and experience to palpate the alignment.
- Beyond the awkwardness, palpating and treating the coccyx can also be very tender. However, that stiffness and tenderness is usually similar to other stiff and tender joints in the body.
- Treatments consist of small but often firm and potentially forceful pushes and pulls to the bone and its articulation to the sacrum and surrounding soft tissues.
In short, it’s a joint like any other, only in an awkward location. But this shouldn’t stop us from treating such an impactful structure!
Do You have a Coccyx Issue and Should You Consider Treatment?
This is by no means an exhaustive list, but here is some food for thought if you think you may have a coccyx issue:
- You have coccyx pain! Anyone who’s had a hard fall or childbirth trauma and experiences coccyx pain should most certainly consider a manual assessment and treatment.
- You have pelvic-floor dysfunction. As previously stated, this means either not enough or too much tone in the pelvic-floor muscles. This can manifest itself in several ways, including pelvic-floor pain, various types of incontinence, and/or sexual dysfunction. More subtle pelvic-floor dysfunction can create general hip, pelvis, and low-back pain.
- Your ‘core is weak.’ If you’ve ever been tested or told your core is weak, or you do a lot of core work yet don’t seem to ever get stronger, a dysfunctional coccyx may be the cause.
- You are really stiff! Significant stiffness, namely around the hamstrings (posterior thigh is usually sciatic nerve and fascia restriction), but also in the back, trunk, and even the neck, may be due to coccyx dysfunction. Again, in folks with this sort of neuro-fascial restriction, no amount of standard stretching improves mobility, and in fact, stretching might make the range of motion and pain worse.
- You have a chronic injury. If you’re dealing with a chronic injury that seems impervious to rest and standard orthopedic treatment, it’s time to consider the coccyx. Either of the core-stability and neuro-fascial mobility factors are enough to cause a persistent chronic injury. Chronic nerve pain is a prime reason to assess and treat the coccyx.
As with ultrarunning, just because something is potentially awkward, difficult, and painful doesn’t mean it’s not worth doing. I began treating the coccyx six-plus years ago, first out of necessity. But when I began to see how it impacted other injuries and overall athletic function, coccyx treatment became an important part of my practice.
If you’re a medical professional, recognize that the tools that are often most painful and awkward are also the most potent. If you’re an ailing runner–perhaps someone who’s had a hard fall, experienced tailbone pain, or simply at wits’ end due to chronic pain and injury–seek out a skilled medical professional who can assess this vital structure.
Call for Comments (from Meghan)
- Have you had a coccyx injury? How did it occur and what did it feel like?
- Have you had a coccyx assessment and adjustment? What was the procedure like and did it help your ailment?
