Despite popular myth, running is not associated with an increased risk for joint issues like osteoarthritis or joint degeneration. However, just like the rest of the population, a percent of us will experience osteoarthritis as we age, with increased risk in heavier individuals, those with a history of joint injury, chronic soft tissue injuries (namely tendon and ligament injuries), certain bony deformities (impingements), certain metabolic diseases like diabetes or hemochromatosis (too much iron), and genetics (which feels like bad luck).
Osteoarthritis can impact any joint in your body, but in runners we worry most about our knees and hips. In this article, we focus on the long term wear and tear on your hips. As osteoarthritis advances and pain limits your ability to do the things you love, you and your medical team might decide a hip replacement is right for you. What does that actually entail, and can you return to running after it? In this article we’ll answer those questions and hear from three runners who have gone under the knife.
What Makes up the Hip Joint and What Happens When a Hip Replacement Is Needed?
Your hip is a ball-and-socket joint. The joint is made up of two main parts: a ball (the femoral head) at the top of your femur (thighbone), which fits into a socket (the acetabulum) in the pelvis. There are additional bands of connective tissue, that help to provide stability to both your femur and pelvis. This complex structure supports your body weight and allows us to walk, squat, run, and do the many activities we enjoy.
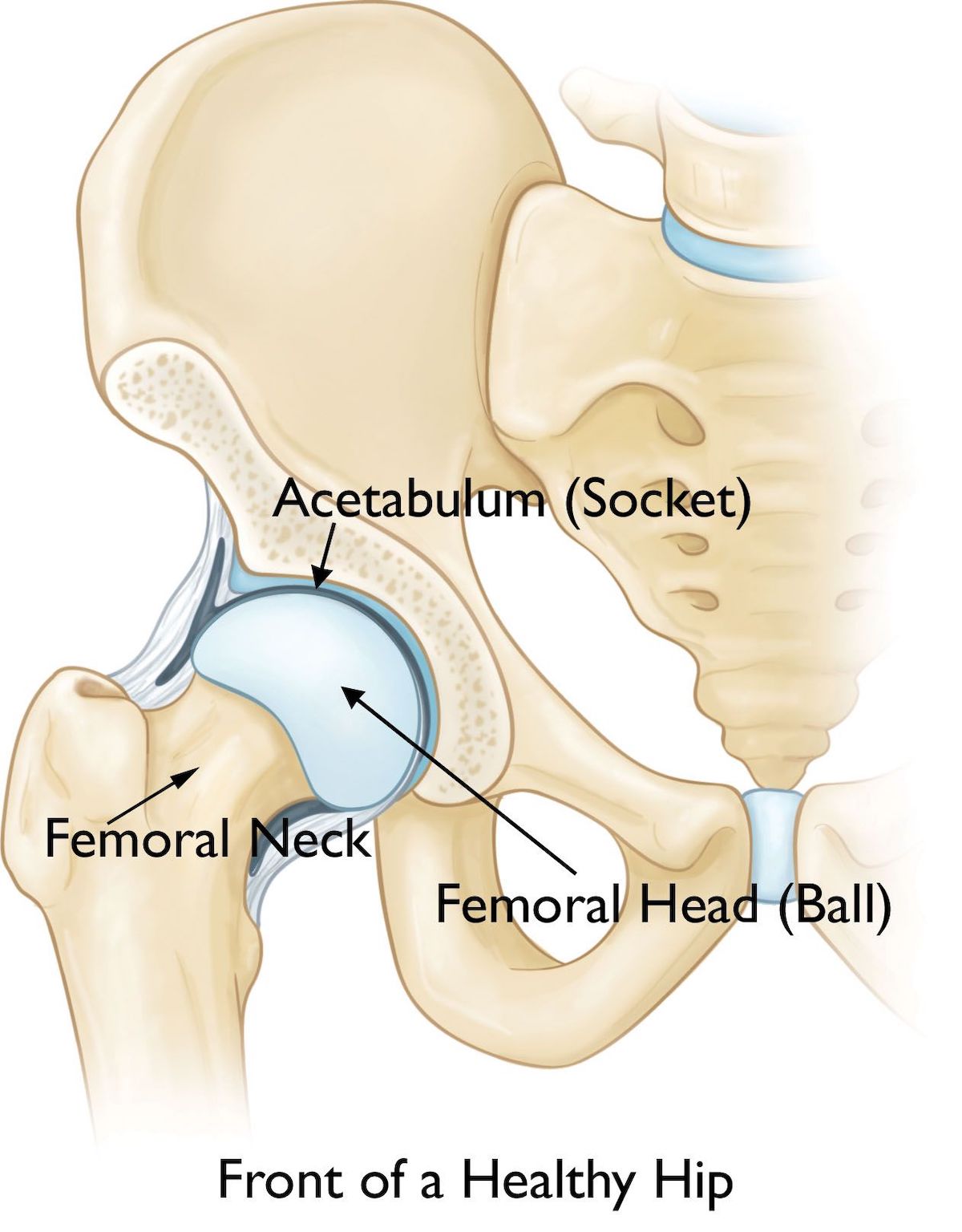
The anterior view of a healthy hip. The femoral head is the ball part of the hip joint, and the acetabulum is the socket. The two together form this ball-and-socket joint. Image: Orthoinfo.aaos.org/en/treatment/hip-resurfacing/
Many conditions may damage the hip joint to the point where replacement is necessary. Rheumatoid arthritis (an overactive immune response resulting in damaged and deformed joints), osteonecrosis (not enough blood supply to the ball portion of your hip resulting in dislocation, fracture, or deformity), and osteoarthritis (wear-and-tear arthritis leading to damaged or deformed joint space) are just some of the culprits. Osteoarthritis is the most common reason a runner might need a hip replacement. Wear and tear of the joint combined with chronic injury creates stiffness and pain.
There is smooth cartilage in the joint allowing the ball and socket to glide over each other with very little friction. However, in osteoarthritis this cartilage is worn down, causing more friction within the joint and even creating bony deformities and growths. These bone spurs further impair joint movement, and the joint space can contain floating bits of bone and cartilage as the wear and tear continues. Not a pretty picture, and often a reason to eventually move onto a surgical intervention.
What Happens When You Have Your Hip Replaced?
There are two types of hip replacements; the one you are likely most familiar with is a traditional total hip replacement (arthroplasty) and the second one (the one I’m most excited about) is called hip resurfacing arthroplasty.
During a traditional hip replacement, the femoral heck and head along with the acetabulum are removed and replaced with metal, plastic, or ceramic components (2).
During hip resurfacing, the femoral neck and head are saved. To preserve this bone, only a thin surface layer of the femoral head is removed and capped with a metal cover, and the same is done for the acetabulum (3). Dr. Thomas Gross, who has performed numerous hip resurfacing procedures including those of Andy Jones-Wilkins, who is interviewed later in this article, said, “Total hip replacement has been called ‘the operation of the century’ because of its dramatic impact on society. But that was the 20th century. Hip resurfacing is the operation for the 21st century (7)!”
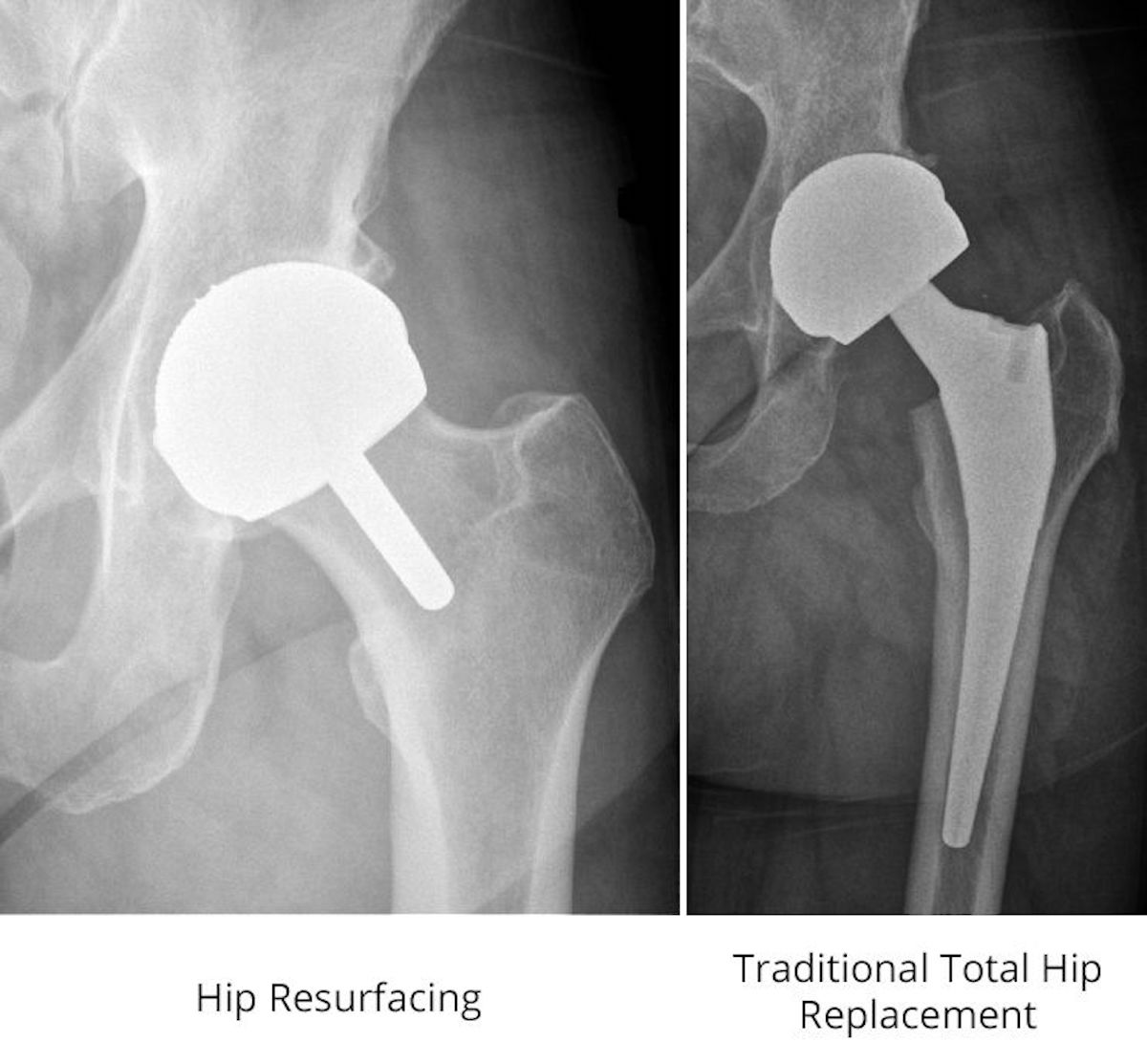
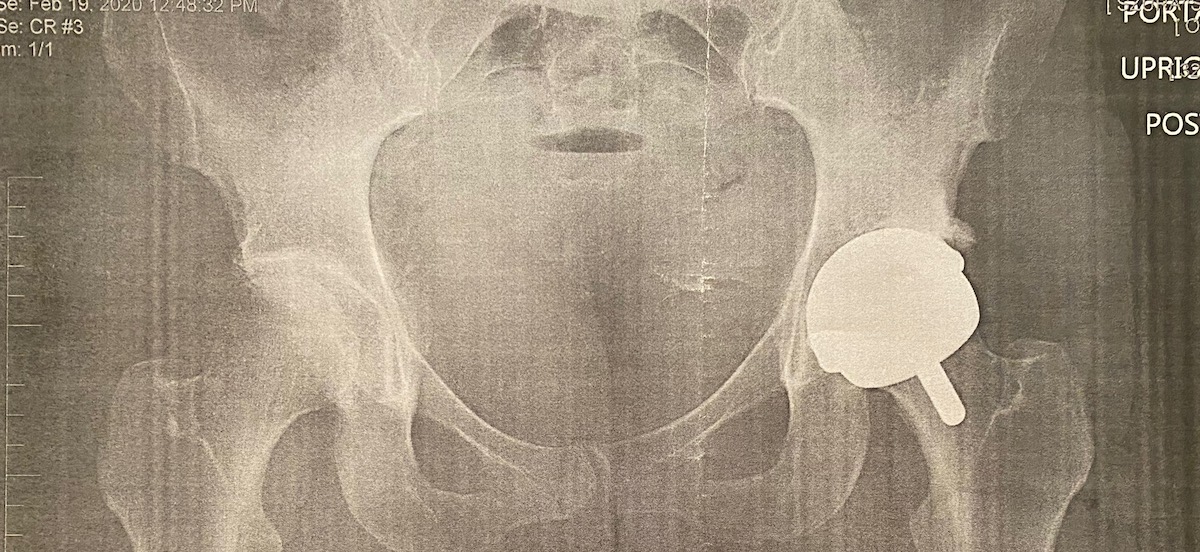
This image shows x-rays of hip resurfacing and traditional total hip replacement. On the left, you can see a resurfaced hip where a metal cap covers the femoral head and a small metal stem extends into the femoral neck. On the right is a traditional total hip replacement where the femoral head and neck are removed and replaced with metal, plastic, or ceramic components. Image: Orthoinfo.aaos.org/en/treatment/hip-resurfacing/
Why Is Resurfacing So Promising for Runners?
While the end results for both total hip replacements and hip resurfacing are generally positive (reduced pain, increased range of motion, and return to activity), hip resurfacing is gaining popularity in more active populations because the surgery allows for better biomechanical reconstruction, preserves the femur (allowing for future revisions), creates less instability, and preserves proprioception (your ability to perceive where your body is in space) (4).
While you can run after both procedures, total hip replacements are at greater risk for loosening and stem fracture with high impact sports and are much harder to repair or revise if they wear out quickly. These things combined seem to make hip resurfacing a really strong alternative to a total hip replacement for individuals under 60 years old who have good bone density and who want to maintain their level of activity for as long as possible.
Literature states roughly 98% of patients return to sports of any impact level after hip resurfacing and 82% return to high impact sports, compared to only 52 to 56% of patients returning to sports after total hip replacement (4).
More recently, a retrospective case study was done looking at eight elite and professional athletes (a baseball, hockey, basketball, and tennis player; an ultramarathon runner; an Ironman triathlete; and an Olympic fencer; all 25 to 64 years old) returning to sport between 2007 and 2017 after hip resurfacing (3). All eight successfully returned to sport at the same level of competition with no post-operative complications. At time of publication in 2021, the fencer had won gold at the Olympics, the tennis player had just retired, and the ultramarathon runner and Ironman triathlete are still competing. While this was a very small retrospective study with only eight subjects reviewed, it is promising to see athletes return to high level and high impact sports post-surgery.
Finally, in a study surveying runners at the UTMB festival of races between 2015 and 2017, researchers found that runners with hip resurfacing were more likely to enter and complete the 100-mile UTMB race than those with a total hip or knee replacement, who more often entered the 50-kilometer OCC or 100k CCC instead. Also, all eight runners in the survey who started UTMB finished the race (6). The study didn’t draw conclusions about completing 100-mile races after joint replacement, but they were encouraged by the response from those who had undergone hip resurfacing.
What About Women and Hip Resurfacing?
Unfortunately, not all patients are candidates for hip resurfacing.
Because hip resurfacing does not remove the head or neck of the femur, the procedure relies on patients having good bone density for the implant to be placed, anchoring it to the bone. Low bone density can rule out both men and women, but females are at higher risk for low bone density compared to males. This is also why the procedure is generally performed on patients under 60 years old. Hip resurfacing is more complicated than a total hip replacement, and doing this procedure on a smaller frame (again, generally women) who require smaller-sized implants is also more complicated.
Smaller size and lower bone density have historically led to higher failure rate of the hip resurfacing in female patients. Specifically, these factors lead to what is called “edge loading,” meaning a mismatch of angle and coverage between the acetabulum cover and the femoral head cover. Not only does this shorten the implants’ lifespan, but it also creates a higher likelihood of chrome and cobalt ions being released (the implants are made of metal) into the surrounding soft tissue, causing painful inflammation.
The medium-term (seven to 10 years post-operation) failure rate for hip resurfacing in women is 8.54 to 11.67%, whereas the same time frame failure rate for a total hip replacement is only 1.81 to 2.25%. This was deemed unacceptably high and so the U.S. Food and Drug Administration pulled smaller implants designed for smaller femoral heads from the market, essentially eliminating that as an option for many females (7). After urging from surgeons, who argued being female should not be an automatic contraindication for surgery and stressed that surgical effort to place the implants better for smaller joints even if more nuanced and more complicated was worthwhile (7), implants came back onto the market.
It can still be difficult to find a surgeon who performs hip resurfacing on female patients. What’s important to recognize is this decision is going to look different for each individual. Ultimately, if you are battling late stage osteoarthritis and are under 60 years old, discussing quality of life versus risk of a revision with your medical team is worth it.
An Interview with Andy Jones-Wilkins
Ultrarunning legend and longtime iRunFar columnist Andy Jones-Wilkins (AJW) answers questions about getting a second opinion on treatment options for osteoarthritis for his left hip, recovering from hip resurfacing of his left hip in 2015 and his right hip in 2018, and his return to running after both.
iRunFar: You’ve had hip resurfacing on both hips and you state this is the reason you can still run ultras. Why resurfacing versus replacement?
AJW: I was diagnosed by a doctor at University of Virginia with end stage arthritis in the spring of 2015. He told me I had no choice but to have a total hip replacement and likely never run again. I began researching hip resurfacing and contacted Dr. Thomas Gross in Columbia, South Carolina in the summer of 2015 after talking to one of his patients who had hip resurfacing in 2013 and then ran the Hardrock 100 in 2014. Dr. Gross asked me to send him my x-rays and said he would get back to me if I was a candidate. A couple weeks later he called and said I was a good candidate (under 60 years of age, good bone density, not overweight, and no femoral head cysts) and in September 2015, I had my left hip resurfaced.
After six weeks I returned for a checkup and was cleared for all activities except running. After six months I was cleared to run. I told Dr. Gross I planned to run Hardrock in July 2016 (it was March at the time) and he said if my hip felt okay he didn’t see any problem with that. I finished Hardrock that year.
iRunFar: Was your medical team understanding of what you wanted to be able to return to?
AJW: Completely understanding. Most of Dr. Gross’s patients are athletes and he has a long list of success stories with runners, skiers, surfers, tennis players, martial arts people, and others. His whole philosophy is that he can repair the joint and it’s up to the patient to do the rest (rehabilitating the muscles, tendons, scar tissue, the whole works). The physical therapy and rehab from the surgeries is like training for an ultra.
iRunFar: Generally speaking, resurfacing seems to be reserved for younger male athletes. Did you discuss age at all?
AJW: I was 47 when I had my left side done. Dr. Gross told me he thought I maybe had two to three years left on my right hip and if it started to act up I should try to get it done before too long. And, sure enough, my right hip deteriorated quickly in the winter of 2017 to 2018 and I had that hip resurfaced in April 2018 when I was 50.
iRunFar: Did the medical team place any return-to-sport limitations on you?
AJW: There were significant limitations in the first six weeks after surgery and moderate limitations until the six-month mark. After that, I had no limitations other than what my body was telling me. Some days are better than others. Dr. Gross left me with one important piece of wisdom after my second surgery, “You will have abnormal anatomy and physiology for the rest of your life and your body will do some strange things. As long as you are prepared for when that happens and you take what your hips allow you to do, then you’ll be fine.”
iRunFar: How was your personal experience in getting back to running after each procedure?
AJW: After my first surgery, I returned to running after six months and felt about 90% normal. My second surgery, which ended up being much more invasive (the surgeon can’t predict until the procedure has started how deep he will need to go and how significantly he will need to dislocate the hip and/or how much of the gluteal muscle he will need to cut through), took me a full 18 months to recover from. After that experience, I certainly felt as though I could no longer run as fast as I once did, especially since over-striding put a strain on my hip flexors. Since then I would say my running has been “normal” as I was able to run over 3,000 miles in 2020, and will probably run about 2,500 in 2021 with quite a bit more vertical. All in all, I am a very satisfied customer.
iRunFar: Were your expectations for post-operative function met?
AJW: Yes, absolutely.
An Interview with Missy Gosney
Missy Gosney’s list of top-five finishes in mountain 100-mile races is long and includes The Bear, Hardrock, Bighorn, and Cascade Crest, but nagging hip injuries eventually led her to undergo a total hip replacement. In this interview, Missy talks about making that decision and what a return to activity has looked like after surgery.
iRunFar: Can you tell me a little bit about your decision to have a total hip replacement?
Gosney: Over the course of a few years, I had [a number of] injuries — iliotibial band, piriformis, psoas, and groin. I spent time and money on physical therapy, massage, and other alternative treatments. I got to a point where I could not sleep at night without rigging ways for my feet to not splay open and I would dismiss comments that I limped. I ran my final 100-mile race the summer prior to visiting an orthopedist. The pain after that 100-mile was beyond anything I had experienced.
I had no idea that all these injuries were related to the deterioration of my hip labrum. By the time I went to an orthopedist, x-rays indicated that I had destroyed my labrum and would need a replacement. My orthopedist sent my x-rays to a labrum repair specialist who determined I was not a candidate for labrum repair because my labrum didn’t exist. [It was] bone on bone. My orthopedist discussed resurfacing versus replacement. I decided on replacement and was in surgery three weeks later. This is a fast time frame from orthopedic [consult] to surgery. Often patients know they need a hip replacement, and get cortisone shots to extend the time to surgery.
iRunFar: It’s my understanding that you are not supposed to run on a hip replacement. How did that conversation go with your medical team?
Gosney: When I decided to get a hip replacement, I was told that I could not run on it.
iRunFar: If you were told that hip resurfacing was not an option for you, was the medical team clear about why a hip replacement was better for you?
Gosney: The conversation with my orthopedist was to determine if I wanted to pursue resurfacing versus replacement. I wanted to have a local surgeon [where I live in Durango, Colorado], an experienced surgeon and a recommended surgeon. My orthopedist had operated on me for a leg fracture three years prior. Resurfacing would allow me to run, but that surgery is a “short term fix.” Eventually resurfacing needs a replacement. [Author’s Note: Not all hips that are resurfaced need to be replaced, but they are easier to revise because of the remaining femoral head and neck]. Both of these are big surgeries. I determined that resurfacing is only done by a few orthopedic surgeons nationwide. It is controversial. I decided the metal-on-metal risks were too high, along with having to travel for the surgery, and not knowing my surgeon.

Missy (left) and Anna Frost at the trailhead after completing the Nolan’s 14 in 2015. Photo courtesy of Anna Frost.
iRunFar: Have you been able to return to run since having your hip replaced?
Gosney: Yes! I am a mountain runner. Mountain running is very different than hauling ass on the bike path. I hit dirt every day – it’s a combination of powerhiking, running, and slow going downhill. I use poles to deflect the impact. I will never run a 100-mile race again. I consider every rotation of my hip one step closer in the life span of my replacement — I want to run every day and not just one big event!
iRunFar: What was the conversation like with your medical team?
Gosney: A good orthopedic [surgeon] has the obligation to discourage running on a hip replacement. Their objective is to get the longest life span out of the prosthetic. My most recent checkup showed excellent durability of my replacement. My surgeon knows I run on my replacement and reminds me that I will not get the same life span out of my hip. I am reminded that a second surgery is not easy. And I run because of the benefits to my overall health!
iRunFar: Have your expectations for post-operative function met?
Gosney: Yes, and beyond! My surgeon has a tremendous amount of experience — he does over 250 hips a year — and it paid off. I think this is the most important part of replacement.
iRunFar: Is there anything you wish you had known going into the procedure?
Gosney: I wish I had visited an orthopedic [surgeon] sooner with the injuries I was experiencing. X-rays are easy to get and show the changes in hips.
iRunFar: Is there anything else I should know?
Gosney: I recommend anyone who is running weekly high volume to get a gait analysis and go to a professional Pilates or deep core instructor to address weaknesses.
An Interview with Sam Szura
Missy Gosney introduced us to Sam Szura, a female runner who was able to get their hip resurfaced. This interview discusses Sam’s athletic history, the long presentation of a chronic hip issues, and how she weighed the decision to ultimately have her hip resurfaced.
iRunFar: Can you give us a glimpse into your athletic background?
Szura: I have been a runner my whole life, high school track and cross country and two seasons of cross country in college. As a senior in high school, I had some left hip pain. During track season, I had a few weeks off and was given a cortisone injection to allow me to finish my track season. [Author’s Note: A cortisone injection is a corticosteroid injected into the joint space to alleviate inflammation.] Fast forward to after college, I would run just to get a quick workout. I did way more step aerobics my last year of college and through my twenties than anything else. I always had some hip flexor pain and knew I had a labral tear by talking with people in the field, but just figured “oh well.”
iRunFar: I understand you went through one procedure before ultimately having your hip resurfaced. What did that look like?
Szura: In 2012 and 2013, I had pretty significant left hip pain while dancing at a party. Suddenly, when I would stand or walk or exercise it would “catch.” I met with Dr. Jennifer Forrest who referred me to a Dr. Brian White in Denver, Colorado. I was told my left hip joint was arthritic. I had a CAM defect, an impingement in which the femoral head is not round and thus cannot smoothly rotate inside the socket, and a shredded labrum.
After meeting with Dr. White and discussing thoroughly cadaver labrum surgery and possible micro-fracture treatment for the left acetabulum, we scheduled surgery for June 2014. That surgery was quite extensive and after rehab I was good for 4.5 years. I was running a couple times a week on the road for three to six miles and all my others activities were aerobic/HITT classes, water skiing, and snow skiing.
In November 2018, I experienced a similar terrible pain in left hip flexor. I spoke with Dr. White, and imaging showed my cadaver labrum was pretty much dead.
iRunFar: So after this initial surgery didn’t survive long term, what did your options look like from there?
Szura: Over the next year, I spoke with several physicians as well as friends that had hip resurfacing versus total hip replacements. I did a cortisone injection to alleviate pain and go on a big ski trip we had planned. During this time, I also contemplated doing platelet-rich plasma injection and ultimately decided it wasn’t going to fix anything, with different results in the U.S. versus abroad. My significant other is a radiologist and we discussed at length what I wanted to get out of surgery. Ultimately, I was at a point where I was tired of dealing with the pain.
There were four or five people in Durango, Colorado where I lived who had had resurfacing done with Dr. Thomas Gross in South Carolina. I spoke with him several times, and spoke with a good friend of mine that had her resurfacing done when I had my cadaver labrum done, and she was still very happy. I finally decided to get the resurfacing surgery because I wanted to run, that’s it.
I was 49 years old when I had my surgery and Dr. Gross has been resurfacing hips for over 15 years. He did stop doing surgery on women for a few years because the implants were too big and as a result some women experienced fractures and the smaller sizes were taken off the market for some time. Dr. Gross was instrumental in getting the smaller implants back on the market and in turn started doing resurfacing on women again.
iRunFar: Once you were finally able to get the surgery, how was your experience post-operatively?
Szura: I think total hip replacements are a very good, very reliable surgery. They are pretty easy to recover from; the down time is next to none; you’re up walking if you are healthy that day!
My rehab was quite a bit slower. There is no physical therapy post-op for hip resurfacing. You are given exercises you do several times a day. They seem so simple but the whole idea is not to flare up the hip flexor. You are weight bearing with crutches, provided your bone density is sufficient, for two weeks. You go to one crutch after that for approximately one week. You can walk 400 yards per day for activity the first week, 800 yards the second week, 1,200 yards the third week, and one mile the fourth week. After that you can start walking more until pain. You cannot ride the bike until six weeks for risk of dislocation.
I bought a portable ice machine and I lived in it to help with swelling. The incision was big at first, crescent shaped along the lateral buttocks. They do a gluteal splitting and then detach and reattach the external rotators and some other things I don’t remember. I would say the incision was the sorest part.
Otherwise, I really had no pain. I took the pain medication as advised the first three days just to get through the long flight home and airport time. Then it was just the aspirin and blood thinner as prescribed.
You aren’t allowed to flex past 120 degrees until your six-week post-op appointment. Any total joint is going to feel weird – you’re swollen, tight, and not able to move naturally for some time.
iRunFar: Now that you are a little more removed from the procedure, how do you feel about the decision to go the route of hip resurfacing?
Szura: Missy Gosney and I have talked many times about our bionic hips. We did two different approaches to ultimately achieve the same outcome. I am essentially pain free, and get a touch of hip flexor tendinitis if I compensate not using my quadriceps, but there is no joint pain. My leg length is great, and gait is great.
The side of my hip had some fat atrophy, which you are told will happen so it’s sometimes uncomfortable to lay right on the prominent part of my hip, but I wouldn’t call it a problem.
People ask if would I do it again, at my age and wanting to run? Yes, 100%. Down the road if my right hip needs replacing, I will most likely do the [total] hip. It’s a shorter surgery and recovery. I won’t be concerned with causing an issue with my implant so I still will run, [but] the running won’t be as fast and long, so the impact will most likely not [be] enough to cause harm.
I found a doctor, Dr. Gross, who had an enormous amount of experience and knowledge, and was well respected for resurfacing. The fact that he stopped operating on women for a while when there were complications and some changes being made with the implants, that really stuck with me. The fact that Dr. Gross operates on a lot of younger, healthy, athletic patients who want to continue their lifestyle post-op was also very important. I work in [the medical field] and I believe that you should do your research. Every patient has specific goals. I am extremely happy I was able to go to Dr. Gross and have a great outcome.
In Summary
While hip resurfacing might be the future of treating osteoarthritic hips in younger active individuals, allowing you to return to activity quicker and for the long haul, it might not be for everyone.
Hip resurfacing is not without its own risks and limitations. Not everyone will be a good candidate for the surgery, and that is a discussion you will have to have with your surgeon and medical team. You can technically run on a total hip replacement, but it’s discouraged as you shorten the lifespan of the implants and are at a higher risk of fracture with high impact activities. That being said, an anterior total hip replacement is a quicker procedure to recover from and is widely done well, making it easier to find a surgeon. Women might be less likely to opt for hip resurfacing due largely to anatomy, but also to the fact that it’s just harder to do, which means less surgeons are willing to take on that risk.
Both surgeries can allow individuals to improve their quality of life by removing pain and improving range of motion (allowing you to move better), but what is best for you is up to you, your medical team, and the cards you’re dealt. Be your own advocate and keep your eyes and ears open for advancements in these procedures.
Call for Comments
- Have you ever had a hip replacement, or have you been told that you may need one in the near future?
- If you have, how has your running and other activities been affected?
- Have you considered hip resurfacing instead, or discussed it with your doctor?
References
- Alentorn-Geli, E., Samuelsson, K., Musahl, V., Green, C. L., Bhandari, M., & Karlsson, J. (2017). The association of recreational and competitive running with hip and knee osteoarthritis: A systematic review and meta-analysis. Journal of Orthopaedic & Sports Physical Therapy, 47(6), 373–390. https://doi.org/10.2519/jospt.2017.7137
- American Academy of Orthopedic Surgeons. (n.d.). Hip resurfacing – orthoinfo – AAOS. OrthoInfo. Retrieved November 1, 2021, from https://orthoinfo.aaos.org/en/treatment/hip-resurfacing/.
- Morse, K. W., Premkumar, A., Zhu, A., Morgenstern, R., & Su, E. P. (2021). Return to sport after hip resurfacing arthroplasty. Orthopaedic Journal of Sports Medicine, 9(5), 232596712110035. https://doi.org/10.1177/23259671211003521
- Girard, J., Miletic, B., Deny, A., Migaud, H., & Fouilleron, N. (2013). CAN patients return to high-impact physical activities after hip resurfacing? A prospective study. International Orthopaedics, 37(6), 1019–1024. https://doi.org/10.1007/s00264-013-1834-4
- Meek, R. M., Treacy, R., Manktelow, A., Timperley, J. A., & Haddad, F. S. (2020). Sport after total hip Arthroplasty: Undoubted progress but still some unknowns. The Bone & Joint Journal, 102-B(6), 661–663. https://doi.org/10.1302/0301-620x.102b6.bjj-2020-0208
- Rochoy, M., Six, J., Favre, J., Lagrange, N., Lefebvre, J.-M., Rollier, J.-C., & Girard, J. (2020). Does hip or knee joint replacement decrease chances to complete an ultra-trail race? study in participants at the ultra-trail du Mont Blanc®. Orthopaedics & Traumatology: Surgery & Research, 106(8), 1539–1544. https://doi.org/10.1016/j.otsr.2020.07.011
- Gross, T. P. (2021). Hip resurfacing: Is female gender an absolute or relative contraindication? Annals of Joint, 6, 23–23. https://doi.org/10.21037/aoj.2020.04.05